Pulmonary Arterial Hypertension (PAH)
Pulmonary Arterial Hypertension (PAH) Treatments:
Welcome to Child Heart Doctors, a team of Pediatric Cardiologists dedicated to Pulmonary Arterial Hypertension (PAH) treatment in Howrah and Kolkata. For an appointment, please call (+91) 91630 48066.
Pulmonary Arterial Hypertension (PAH) in Children: Expert Care for a Complex Condition
Pulmonary Arterial Hypertension (PAH) is a complex and serious condition, and as a parent, hearing this diagnosis for your child can be incredibly worrying. At [Your Clinic Name], our team of dedicated child heart doctors specializes in understanding, diagnosing, and managing the unique challenges of PAH in children. We are here to offer advanced expertise, compassionate support, and the most innovative treatments, ensuring your child receives the best possible care for this challenging condition.
We understand the questions and anxieties you may have, and we are committed to explaining every step of your child’s journey in a clear, understandable, and supportive way.
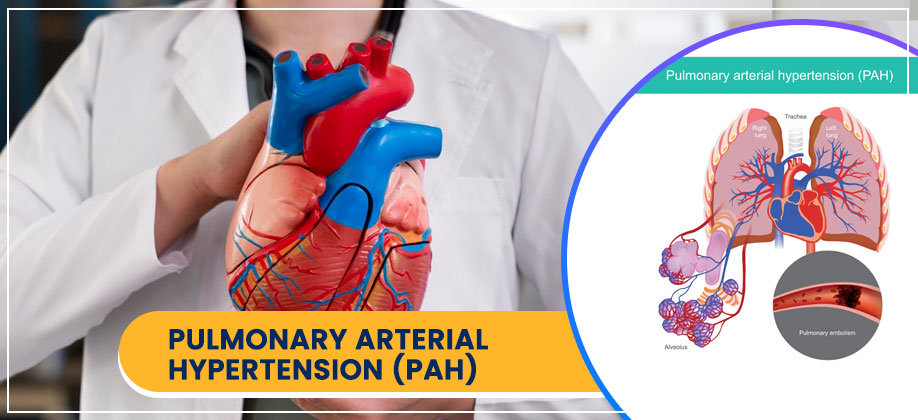
What is Pulmonary Arterial Hypertension (PAH)?
PAH is a type of high blood pressure that specifically affects the arteries in the lungs (pulmonary arteries). These arteries carry blood from the right side of the heart to the lungs. In PAH, these arteries become narrowed, stiff, or even blocked.
How it affects the heart and body:
- Increased Workload for the Heart: When the pulmonary arteries are narrowed, the right side of the heart has to work much harder to push blood through them to the lungs.
- Right Heart Strain: Over time, this extra effort can cause the right ventricle (the heart’s lower right chamber) to weaken and enlarge, leading to right-sided heart failure.
- Reduced Oxygen Delivery: The lungs may not be able to get enough blood to pick up oxygen effectively, leading to symptoms like shortness of breath and fatigue.
What Causes PAH in Children? (Types of PAH)
PAH in children can have various causes, and understanding the underlying reason is crucial for effective treatment. We often categorize it by its origin:
- Idiopathic PAH (IPAH): This means the cause is unknown. It’s diagnosed after all other potential causes have been ruled out.
- Heritable PAH (HPAH): This form runs in families and is caused by specific genetic mutations.
- PAH Associated with Other Conditions: This is a very common type in children and can be linked to:
- Congenital Heart Defects (CHDs): Especially those that cause too much blood flow to the lungs from birth (e.g., large VSDs, PDA, AV Canal defects). If these aren’t repaired, or even sometimes after repair, the lung arteries can become damaged over time.
- Lung Diseases: Such as chronic lung disease of prematurity (BPD).
- Certain Genetic Syndromes: Like Down syndrome.
- Other Conditions: Including certain liver diseases, or connective tissue diseases.
Symptoms of PAH in Children
The symptoms of PAH can be subtle at first and often worsen as the condition progresses. They can also be mistaken for other common childhood illnesses, making early diagnosis challenging. It’s important to pay attention if your child experiences:
- Shortness of Breath: Especially during activity, play, or even crying in infants. They might seem to tire quickly or be unable to keep up with peers.
- Fatigue & Weakness: Unusual tiredness or low energy.
- Chest Pain: Can occur due to the strain on the heart.
- Fainting or Dizziness: Especially during physical exertion. This is a serious symptom and requires immediate medical attention.
- Bluish Tint to Lips or Skin (Cyanosis): Particularly during activity or crying, indicating low oxygen levels.
- Swelling (Edema): In the ankles, feet, legs, or abdomen due to fluid buildup.
- Heart Palpitations: Feeling like the heart is racing or pounding.
- Poor Growth or Weight Gain (in infants and younger children).
Detailed Workup & Diagnostic Procedures
Diagnosing PAH accurately requires a thorough and specialized evaluation. Our team uses a comprehensive approach to confirm the diagnosis, determine its cause, and assess its severity.
- Thorough Medical History & Physical Exam: We’ll carefully discuss your child’s symptoms, their medical history, any family history of heart or lung conditions, and perform a detailed physical examination, including listening to their heart and lungs, checking for swelling, and assessing for any bluish discoloration.
- Echocardiogram (Echo): This non-invasive ultrasound of the heart is often the first and most important test. It helps us estimate the pressure in the pulmonary arteries and assess the function of the right side of the heart. While it can suggest PAH, it cannot definitively diagnose it.
- Electrocardiogram (ECG or EKG): Records the electrical activity of the heart, showing signs of right heart strain or enlargement.
- Chest X-ray: Can show enlarged pulmonary arteries or an enlarged right ventricle.
- Blood Tests: To look for underlying causes (e.g., autoimmune conditions, genetic markers) and assess overall health.
- Pulse Oximetry: Measures oxygen levels in the blood, which can be low in PAH.
- Cardiac MRI/CT Scan: Provide detailed images of the heart, lungs, and blood vessels, helping to identify structural issues or assess the extent of the disease.
- Right Heart Catheterization (RHC) – The Gold Standard:
- What it is: This is the most accurate test for diagnosing PAH and determining its severity. A thin, flexible tube (catheter) is gently guided through a vein (usually in the leg or neck) into the heart’s right side and into the pulmonary arteries.
- How it helps: It directly measures pressures in the heart chambers and pulmonary arteries, blood flow, and oxygen levels. During the procedure, we can also test how the pulmonary arteries respond to certain medications (vasoreactivity testing) to help guide treatment.
- Why it’s important: RHC provides crucial information that non-invasive tests cannot, allowing us to accurately classify the PAH and tailor treatment.
- Pulmonary Function Tests (PFTs): To assess lung capacity and function.
- Genetic Testing: May be recommended if HPAH is suspected or to understand the genetic basis of a child’s condition.
Comprehensive Treatment & Complex Interventions
- General Support & Medications:
- Oxygen Therapy: If blood oxygen levels are low.
- Diuretics: To reduce fluid buildup.
- Anticoagulants: To prevent blood clots in the pulmonary arteries.
- PAH-Specific Medications: These are critical and work to relax and widen the pulmonary arteries, reducing the pressure. They can be given orally, inhaled, or continuously intravenously (IV) or subcutaneously. Examples include:
- Endothelin Receptor Antagonists (ERAs)
- Phosphodiesterase-5 (PDE5) Inhibitors
- Prostacyclin Analogues (e.g., epoprostenol, treprostinil)
- Soluble GuanylateCyclase (sGC) Stimulators
- Complex Interventions:
For some children with severe PAH or specific types of underlying heart conditions, specialized procedures may be considered:- Atrial Septostomy (InteratrialSeptal Stenting):
- What it is: This is a palliative (symptom-relieving) procedure for select children with very severe PAH and failing right heart function. A small hole is created or enlarged in the wall between the two upper heart chambers (atrial septum), sometimes kept open with a stent.
- How it helps: By creating a controlled "right-to-left" shunt, it allows some blood from the high-pressure right side to bypass the lungs and reach the left side of the heart, which can improve oxygen delivery to the body and reduce strain on the failing right ventricle. It can provide a temporary bridge while awaiting other treatments or transplant.
- Why it’s complex: It requires careful patient selection and expert execution due to the delicate balance of pressures.
- PDA Stenting (for certain complex congenital heart defects with PAH):
- What it is: In some very specific and rare situations, particularly in newborns with certain types of complex congenital heart disease (like pulmonary atresia with intact ventricular septum and severe PAH), maintaining an open PDA (Patent DuctusArteriosus) with a stent can be a strategy. This is not for typical PAH, but for complex, "duct-dependent" heart conditions where the PDA is needed to provide lung blood flow or systemic blood flow.
- How it helps: It ensures reliable blood flow for the child’s survival and growth until definitive repair is possible or other treatment strategies for PAH are established.
- Surgical Repair of Underlying Defects: If PAH is caused by a large congenital heart defect that can be corrected (e.g., a large VSD), surgical closure of the defect is often performed. This aims to reduce the excessive blood flow to the lungs and prevent further damage to the pulmonary arteries.
- Transcatheter POTT shunt creation: creating a communication between aorta and pulmonary artery for symptomatic improvement. This is a highly complex procedure which requires specialexpertercise done by child heart doctors.
- Atrial Septostomy (InteratrialSeptal Stenting):
- Lung or Heart-Lung Transplant: For children with end-stage PAH who do not respond to other therapies, lung transplantation (or heart-lung transplantation) may be the ultimate treatment option. This is a highly complex procedure performed at specialized transplant centers.
Our Commitment: Collaborative and Compassionate Care
Managing PAH is a long-term journey that requires a dedicated team. Our pediatric cardiologists work closely with pulmonologists, critical care specialists, geneticists, nurse coordinators, social workers, and other allied health professionals to provide comprehensive, multidisciplinary care.
We are committed to:
- Early and Accurate Diagnosis: Using advanced techniques to understand your child’s unique condition.
- Individualized Treatment Plans: Tailoring therapies to achieve the best possible outcomes.
- Ongoing Monitoring: Regular follow-ups to adjust medications and manage disease progression.
- Family-Centered Support: Providing education, resources, and emotional support to your family every step of the way.
If your child has been diagnosed with Pulmonary Arterial Hypertension, or if you have concerns about their symptoms, we are here to offer our specialized expertise and support.
All Services:
- Fetal Cardiology
- Pediatric Arrhythmia Management
- Interventional Cardiology
- Cardiac Imaging Service
- Congenital Heart Defects
- Acquired Heart Conditions
- Symptoms & Diagnosis of Heart Conditions in Children
- Congenital Muscular Dystrophy (CMD)
- Heart Failure in Children
- Pulmonary Arterial Hypertension (PAH)
- Congenital Heart Disease
- Special Heart Tests for Children
- Special Heart Interventions for Children
For Appoinment Call
(+91) 91630 48066