Preterm PDA Closure: A case study of a premature infant with a large, medically unresponsive patent ductus arteriosus (PDA) successfully treated with a percutaneous device by a group of child heart doctors in Howrah, West Bengal, resulting in improved cardiac and respiratory function.
Case Summary
This case study details the successful management of a preterm infant with a persistent, hemodynamically significant patent ductus arteriosus (PDA) that was unresponsive to medical treatment. The patient was a 1.8 kg baby with a gestational age of 32 weeks. After being born at an outside hospital, the infant was transferred to Narayana Health Hospital in Howrah for further evaluation and management due to a persistent need for non-invasive ventilation (NIV). The infant had already undergone three courses of paracetamol (PCM) and one course of a non-steroidal anti-inflammatory drug (NSAID) in an unsuccessful attempt to close the PDA medically.
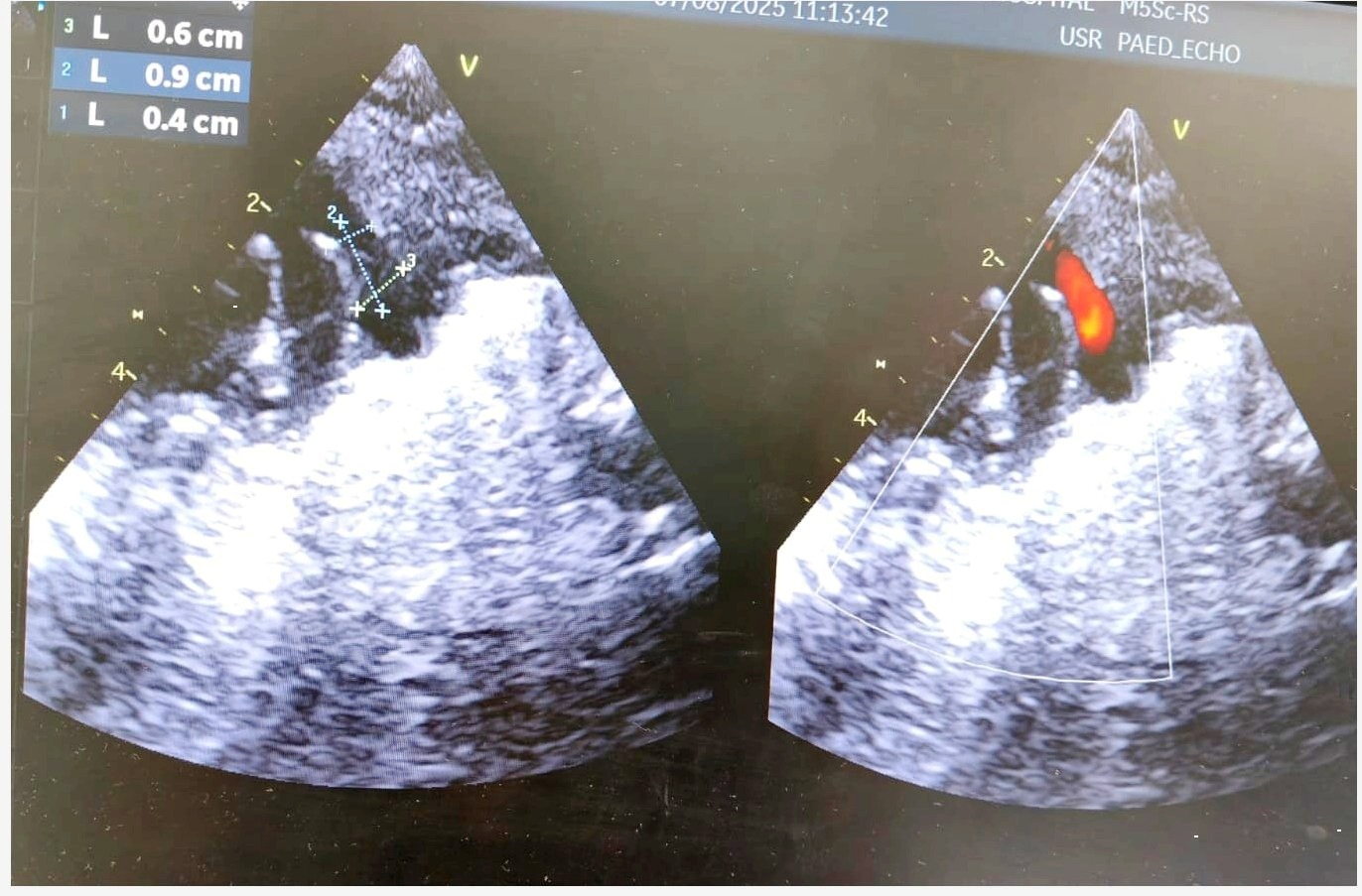
Diagnosis
Upon admission, a chest X-ray revealed cardiomegaly and pulmonary plethora, consistent with fluid overload from left-to-right shunting. An echocardiogram confirmed the presence of a hemodynamically significant PDA, classified as Type F. The ductus arteriosus had a wide opening with specific measurements: an aortic end of 6 mm, a pulmonary artery (PA) end of 4 mm, and a length of 9 mm.
Line of Treatment
Due to the failure of medical management and the persistent need for respiratory support, a percutaneous device closure was chosen as the definitive treatment.
- Preparation: The infant was electively intubated and taken to the cardiac catheterization lab.
- Procedure: A single access was obtained via the right femoral vein (RFV). A 5 x 2 mm Piccolo device was used for closure and deployed intraductally.
- Post-Procedure Management: Immediately following the procedure, the infant developed severe left ventricular (LV) dysfunction, likely due to an afterload mismatch. This was managed with intravenous infusions of levosimendan and dobutamine.
Results
The device successfully closed the PDA without any post-procedural complications such as left pulmonary artery (LPA) obstruction or coarctation of the aorta. The severe LV dysfunction was managed effectively, and the infant was extubated just two days after the procedure. The inotropic support was weaned off, and the baby was discharged 10 days post-procedure with mild residual LV dysfunction. At a follow-up visit 15 days later, the baby was doing well, and their condition had significantly improved.
Read Also: