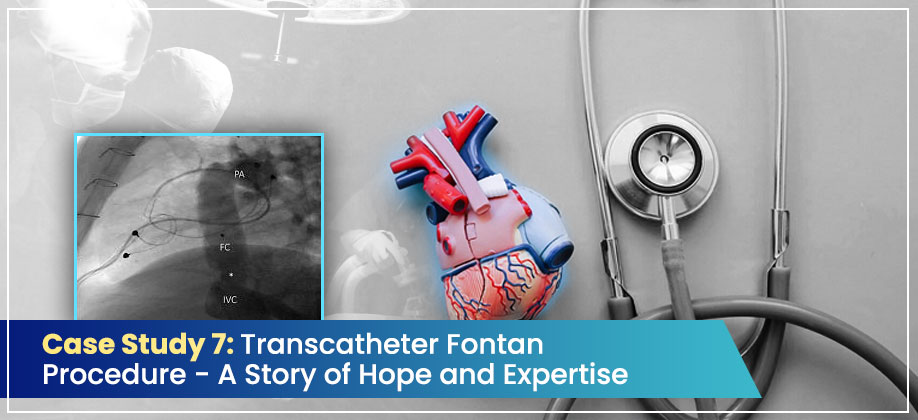
This is the story of our third successful Transcatheter Fontan procedure at Narayana Health Hospital, Howrah. It’s a story of an 11-year-old girl, a testament to her family’s faith, and the tireless dedication of our team.
Case Summary
An 11-year-old girl, with a spirit much bigger than her 26.5 kg frame, came to us seeking a Fontan completion. She had been on a long journey, starting at just one year of age when she underwent a bilateral BD Glenn shunt and an LPA plasty to manage her Tricuspid atresia IIB. Despite her challenges, she was a fighter. Her recent cardiac catheterization brought good news, showing normal PA pressure and PVRI—the green light we needed for a Fontan. However, we also found multiple PAVMs in her right lung, a complicating factor we were prepared to address.
Diagnosis
Our young patient’s diagnosis was Tricuspid atresia with PAVMs. Tricuspid atresia is a complex congenital heart condition, and the prior surgeries were a brave first step. The presence of pulmonary arteriovenous malformations, which are abnormal vessel connections in her lungs, added another layer of complexity to her case, requiring our full attention and a meticulous plan.
Line of Treatment
Our brilliant team decided on a transcatheter Fontan procedure, a less invasive approach that meant a faster recovery for our young patient. Using a single Xephyr CS covered stent, 69 mm in length, we approached the procedure through her existing left Glenn shunt. A key part of our strategy was to create an in vitro fenestration—a small, controlled opening in the stent—which would help her heart adjust to the new circulation pattern. This careful planning, led by our eminent leader Dr. Amitabha Chattopadhyay, and meticulously executed by Dr Jayita Nandy Das, Dr. Rishika Mehta and Dr. Anwesha Mukherjee, our vibrant new team member, made all the difference.
Results
The outcome was truly heartwarming. Our little patient was a superstar. She was extubated on the very same day of the procedure with minimal support, a clear sign of her body’s incredible resilience. There were no post-operative effusions, and her journey to recovery was remarkably smooth. Just six days later, she walked out of the hospital, discharged with a stable SpO2 of 92%, and a new lease on life, ready to embrace a brighter future. She went home with a prescription for Ecosprin and warfarin, but more importantly, she left with a sense of hope and a smile that lit up the entire hospital floor. This was a true team effort, and we are incredibly proud of what we achieved together.
Read Also:
- Case Study 6: Neonatal Ductal Stenting – A Bridge to Life
- Case Study 5: RVOT Stenting for DILV with DORV and Trickle Flow
Read all Case Studies. Follow us on Facebook